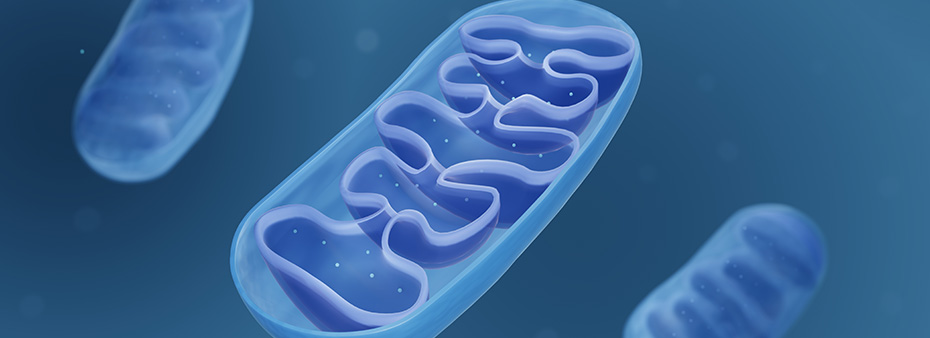
Mitochondrial dysfunction is associated with the development of some of the most common cardiac conditions we manage—atherosclerosis, ischemia-reperfusion injury, hypertension, diabetes, cardiac hypertrophy, heart failure and arrhythmia. Due to the high energy demands of cardiac cells, mitochondria are highly concentrated in these tissues, producing 6 kg of ATP daily through oxidative phosphorylation.
Mitochondrial Health and Cardiometabolic Risk
Interestingly, these powerful organelles also regulate oxidative stress, cell survival and apoptotic death. Therefore, to maintain the integrity of healthy heart structures and the proper utilization of cardiac nutrients, it is imperative to understand how to keep our mitochondria active and undamaged.
Here’s a quick summary of important considerations when managing your cardiometabolic patients.
Mitochondrial DNA Mutations
Mitochondrial DNA is especially prone to oxidative damage since it lacks histones and has a minor capacity for repair. Mitochondrial DNA mutations trigger the induction of a vicious cycle of ROS production. Excessive ROS creates many pathways for increased cardiovascular risks.
- ROS can react with cell components, such as polyunsaturated fatty acids, proteins, nucleic acids, and carbohydrates, which violates the normal properties of cell membranes (such as efficient ion transport), changes enzyme activity, and interferes with protein synthesis and transport.
- ROS-related damage impairs endothelial nitric oxide (NO) synthase, thereby reducing NO-mediated dilatation.
- Oxidative stress provokes the expression of several pro-inflammatory molecules in several models of hypertension.
- The unopposed production of ROS elicits decreased NO synthesis in diabetic hearts, which results in structural alterations of cardiac proteins that negatively affect cardiac muscle relaxation and diastolic dysfunction in diabetic mice.
- Mitochondrial DNA damage of leukocytes is associated with the existence of vulnerable plaques.
- Both prolonged ischemia and acute ischemia-reperfusion injury exert their damage through ROS formation. Total damage is mediated by increased fibrosis, angiogenesis and vascular remodeling.
- Decreased activity of antioxidant enzymes and oxidative modification of cellular compartments is associated with damage in the heart, the brain, the kidneys and the vessels.
Mitochondrial Dysfunction
Mitochondrial dysfunction creates many pathways for increased cardiovascular risks.
- Hypertension is associated with structural mitochondrial abnormalities, which involve decreased mitochondrial mass and density that result in impaired energy production and accelerated formation of ROS through instability of electron transport chain complexes.
- Impaired mitochondrial function is linked to altered glucose and fatty acid metabolism, lower ATP production in muscle cells, impaired insulin secretion from β-cells, and stimulation of ROS production.
- The atherogenic effects of smoking are mediated by oxidative damage to mitochondrial DNA and loss of mitochondrial membrane potential.
- Under conditions of mitochondrial dysfunction, excessive production of ROS contributes to inflammatory vascular reactions, leading to the development of atherosclerotic lesions.
The Bottom Line
The above only begins to delineate what we understand about the relationship between mitochondrial health and cardiometabolic risk. Knowing these varied mechanisms, we can leverage both lifestyle and supplement solutions to either maintain mitochondrial dynamics for prevention or target mitochondrial dysfunction and oxidative stress as treatment. Either way, appreciating the transformational role we can play by supporting mitochondrial health, ATP production and antioxidant reserves is key to reducing one of the world’s leading causes of death.
References
- Panth N, Paudel KR, Parajuli K. Reactive Oxygen Species: A Key Hallmark of Cardiovascular Disease. Adv Med. 2016;2016:9152732.
- Poznyak AV, Ivanova EA, Sobenin IA, Yet SF, Orekhov AN. The Role of Mitochondria in Cardiovascular Diseases. Biology (Basel). 2020;9(6):137. Published 2020 Jun 25.
- Siasos G., Tsigkou V., Kokkou E., Oikonomou E., Vavuranakis M., Vlachopoulos C., Verveniotis A., Limperi M., Genimata V., Papavassiliou A.G., et al. Smoking and atherosclerosis: Mechanisms of disease and new therapeuticapproaches. Curr Med Chem. 2014;21:3936–3948.
- Siasos G, Tsigkou V, Kosmopoulos M, et al. Mitochondria and cardiovascular diseases-from pathophysiology to treatment. Ann Transl Med. 2018;6(12):256.