Dysautonomia has received increased attention over the last few years due to its frequent manifestation in long-COVID patients.1,2 Dysautonomia is a non-specific diagnosis as it is an umbrella term used for any malfunction of the autonomic nervous system (ANS).3 To review, the ANS has two branches: the sympathetic, “fight-or-flight” division and the parasympathetic, “rest-and-digest” division.
Dysautonomia is also known as autonomic dysfunction or autonomic nervous system disorder.4 The clinical manifestations of dysautonomia can be localized or systemic depending on the underlying cause of the condition,3 but it typically involves a dominance of the sympathetic nervous system.5 The ANS performs vital body functions that unconsciously control actions of major organ systems, such as the nervous, circulatory, respiratory, endocrine, digestive and excretory systems.6
Dysautonomia Symptoms
The symptoms of dysautonomia can be so varied and seemingly disconnected that recognizing dysautonomia in the clinical setting can be challenging. Advanced dysautonomia involving postural orthostatic tachycardia syndrome (POTS) and orthostatic hypotension are easier to recognize as the symptoms typically present more severely.
Prior to progressing to severe forms, minor signs and symptoms could exist that indicate the developing problem, such as heart rate variability, occasional lightheadedness when moving from sitting to standing, and chronic anxiety (a sign of sympathetic overdrive). The other symptoms of dysautonomia can present in such a way that it can look like other conditions or a variety of concurrent conditions.
Below is a list of dysautonomia symptoms, although it may not be comprehensive. I have categorized the symptoms for readability, but some could belong in multiple categories (i.e., dizziness can be a blood flow or a head and neck symptom).
Constitutional symptoms
- Fatigue
- Intolerance to heat or cold4
- Insomnia2
Cardiac/blood flow symptoms
- Heart rate variability1
- Palpitations
- Abnormal sweating
- Vasomotor symptoms (hot flashes)
- Hair, skin or nail changes2
Head and neck symptoms
- Brain fog
- Difficulty concentrating
- Dizziness4
- Migraines7
- Vertigo
- Syncope
- Physical instability4
- Hypersensitivity to light
- Blurred vision
- Dry mouth or eyes
- Dysphagia
- Drooling2
- “Coat-hanger pain” (pain in the suboccipital and paracervical region that worsens when upright and relieves when lying down)5
Gastrointestinal/genitourinary symptoms
- Constipation
- Diarrhea6
- Nausea
- Abdominal pain
- Bloating7
- Sexual dysfunction
- Bladder dysfunction2
A patient with dysautonomia would certainly not have all the symptoms listed. The symptoms experienced depend on the location of the autonomic dysfunction. The ANS can be systemic or localized to areas like the heart, cervical chain, adrenal glands, etc.
Most commonly, patients with dysautonomia present with chronic fatigue and symptoms of poor blood flow and tissue hypoperfusion.4 Many of us in practice have probably had patients that were “never well” since a COVID-19 infection, which is thought to be—at least in part—due to dysautonomia and endothelial dysfunction.9,10
Dysautonomia Causes
The underlying cause(s) of dysautonomia can be numerous, although they cannot always easily be determined. Some of the causes of dysautonomia include:
- Chronic stress or an acute stress event
- Diabetes8
- Trauma
- Nutritional deficiencies (vitamins E, B1, B3, B6 and B12)
- Digestive disorders (Crohn’s disease, ulcerative colitis and celiac disease)3
- Viral infections (hepatitis C, HIV, EBV and COVID-19)1
- Ehlers-Danlos syndrome3
- Parkinson’s disease
- Alcohol use disorder1
- Many other causes3
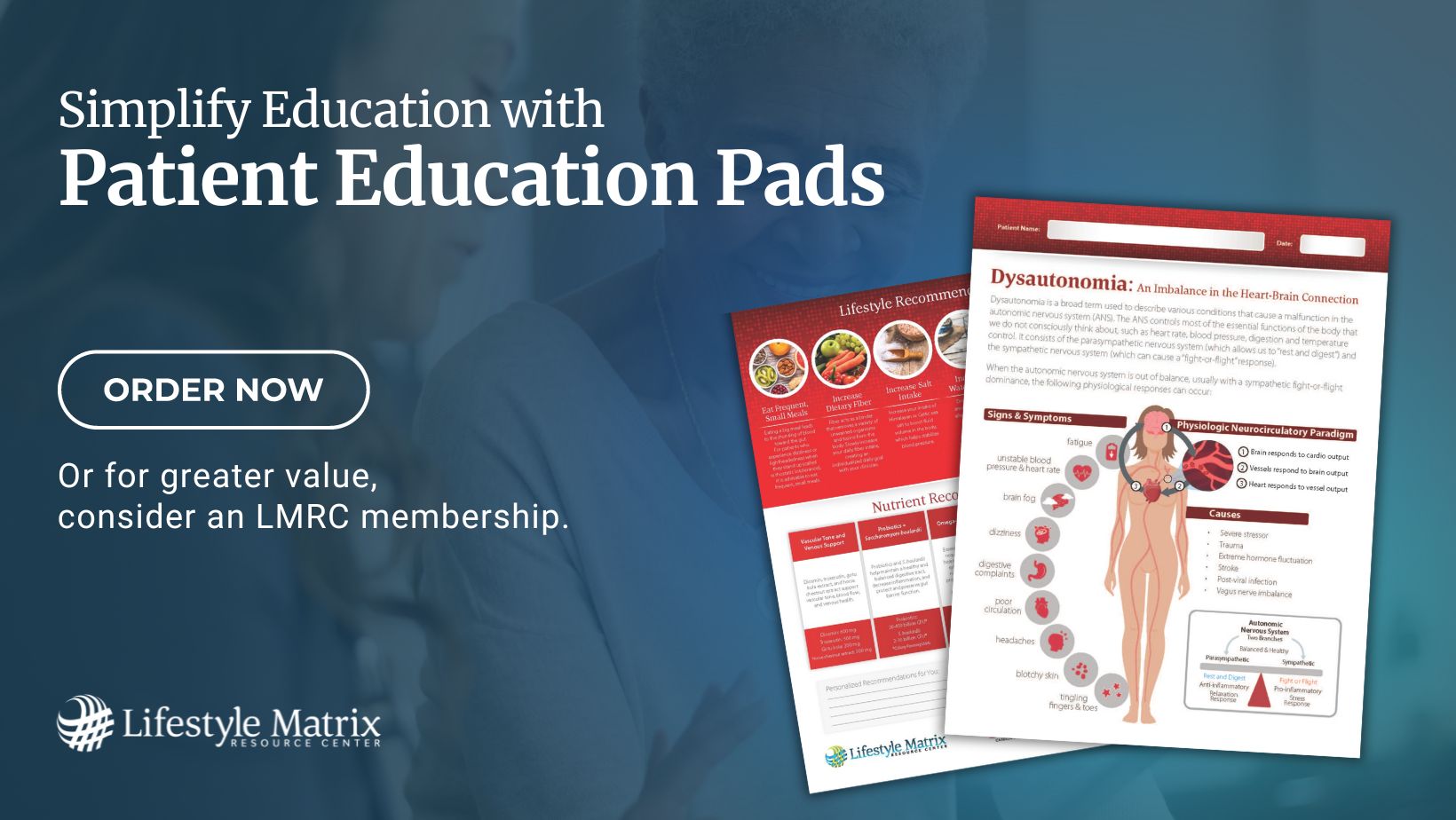
Helping Your Patients Manage Dysautonomia
Dysautonomia management should always focus on treating any pre-existing, underlying cause(s) as this alone can often relieve symptoms.3 There are specific therapeutic recommendations for POTS and orthostatic hypotension that I will not review in this blog post, but recommendations from other articles are available below in the references section.
My personal approach to any dysautonomia patient case would be to address the underlying cause. It is also essential to simultaneously support microcirculation, address any endothelial dysfunction, and promote the body’s healing process with adaptogenic herbs, such as ginseng, licorice root, Rhodiola rosea or ashwagandha.
The Bottom Line
Dysautonomia is a complex yet better-recognized concern since the COVID-19 pandemic. Due in part to the increased attention on the condition, resources for managing dysautonomia continue to emerge throughout the literature. Always consider dysautonomia
in your differential diagnosis in patients who present with fatigue, dizziness, temperature control imbalances, gastrointestinal complaints, and signs of poor blood flow regulation. 
Megan Borreson, ND is the CM Vitals Clinical Brand Manager at Lifestyle Matrix Resource Center. She attended undergraduate school at the University of Wisconsin–Eau Claire and received her Bachelor of Science degree in cell biology and a Bachelor of Arts degree in Spanish with a minor in chemistry. Dr. Borreson then enrolled at National University of Health Sciences where she graduated summa cum laude with a Master of Acupuncture and Doctorate of Naturopathic Medicine.
References
1. Barizien N, Le Guen M, Russel S, Touche P, Huang F, Vallée A. Clinical characterization of dysautonomia in long COVID-19 patients. Sci Rep. 2021;11(1):14042. doi:10.1038/s41598-021-93546-5
2. Finsterer J. Small fiber neuropathy underlying dysautonomia in COVID-19 and in post-SARS-CoV-2 vaccination and long-COVID syndromes. Muscle Nerve. 2022;65(6):E31-E32. doi:10.1002/mus.27554
3. Underlying Causes of Dysautonomia. Dysautonomia International. Published 2019. Retrieved March 7, 2023, from https://dysautonomiainternational.org/page.php?ID=150.
4. Aguirre-Chang G, Trujillo A. Pots, Orthostatic Hypotension and Other Symptoms of Dysautonomia Are Associated with Endothelial Dysfunction, Reduced Blood Flow and Persistent Microclots. Research Gate. 2021.
5. Ricci F, De Caterina R, Fedorowski A. Orthostatic Hypotension: Epidemiology, Prognosis, and Treatment. J Am Coll Cardiol. 2015;66(7):848-860. doi:10.1016/j.jacc.2015.06.1084
6. Do T, Diamond S, Green C, Warren M. Nutritional Implications of Patients with Dysautonomia and Hypermobility Syndromes. Curr Nutr Rep. 2021;10(4):324-333. doi:10.1007/s13668-021-00373-1
7. Olshansky B, Cannom D, Fedorowski A, et al. Postural Orthostatic Tachycardia Syndrome (POTS): A critical assessment. Prog Cardiovasc Dis. 2020;63(3):263-270. doi:10.1016/j.pcad.2020.03.010
8. Eldokla AM, Mohamed-Hussein AA, Fouad AM, et al. Prevalence and patterns of symptoms of dysautonomia in patients with long-COVID syndrome: A cross-sectional study. Ann Clin Transl Neurol. 2022;9(6):778-785. doi:10.1002/acn3.51557
9. Libby P, Lüscher T. COVID-19 is, in the end, an endothelial disease. Eur Heart J. 2020;41(32):3038-3044. doi:10.1093/eurheartj/ehaa623
10. Jung F, Krüger-Genge A, Franke RP, Hufert F, Küpper JH. COVID-19 and the endothelium. Clin Hemorheol Microcirc. 2020;75(1):7-11. doi:10.3233/CH-209007